An insight into the history of pain relief – from death rattle to tears of joy.

Overseas
The filthy lecture theatre, dimly lit by a few lamps, is filled with the nauseating smell of blood and oozing excretions, the quiet, fearful whimpering of the patient waiting for an operation, and the excited murmurs of student surgeons waiting for Warren, the celebrity surgeon of the age. The next show is an amputation, show here being the appropriate word.
The observing medics, particularly the most junior, are gleefully waiting to see which among them will faint first, unable to cope with the patient’s screams, his writhing in agony beneath the ropes, and eventually, probably, his final, horrified death rattle.
Every operation was a sensational, hellish show both for the barbers – later surgeons – and for the observing students.
Effective and widely used anaesthesia was a concept unknown to the whole of humanity until the 16th of October, 1846.
For thousands of years, operations meant the inseparable union of steel and pain. The majority of patients died of the unbelievable shock caused by their suffering, and for those who survived there was sepsis, leaving only a few with fortunate constitutions.
According to histories of medicine, there were altogether 43 operations registered at the Massachusetts General Hospital between 1821 and 1823.
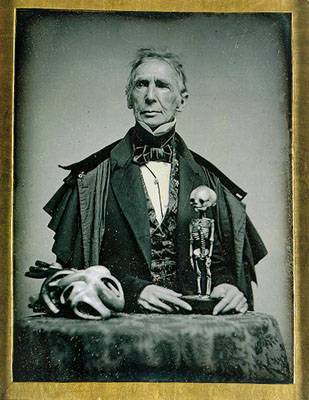
John Collins Warren, professor of anatomy and surgery at the Harvard University Medical School, performed operations at this hospital, coolly amputating conscious patients’ heavily damaged or infected limbs, cutting out their cancerous organs, then wiping his hands on his bloody apron, awaiting his next victim. The elementary importance of handwashing had not yet been discovered.
Trepanation of the skull, amputations, the removals of tumours were done with the patients fully conscious, the little balls suffused with numbing plant extracts used at the time having little effect on the patient’s pain.
Routinely seeing the immeasurable suffering of their unfortunate patients taught surgeons to be unkind and without sympathy. To go under the surgeon’s knife one had to undergo the most abject horrors, where even likely death must have seemed better than one’s current suffering.
Much like most famous and not so famous surgeons at the time, Warren did not believe it possible to operate without suffering, since pain had always been part of operations.
Nevertheless, this haughty, standoffish surgeon, one of the most famous in the world at the time, allowed a man named William T. G. Morton (who had stolen the technique of anaesthesia using ether from its discoverer, Horace Wells) to demonstrate the effects of ether as an anaesthetic. He commented on the day: “During today’s operation we shall try Mr Morton’s new drug, of which they say it miraculously renders those who breathe it in immune to pain.”
Several of his famed colleagues were in attendance that day to watch the ‘miraculous’ intervention, which, whether successful or not, was to involve an operation on Gilbert Abbott, whose lung cancer had spread to his tongue and glands in his chest. The plan for the operation was to extract the tumour, whether the patient was to feel pain or not.
Warren was right to be doubtful on this occasion, since he had met Wells (the true first discoverer of the effects of ether) before, in January 1845. Then, also with permission from Warren – who despite his seriousness and his distant, scornful demeanor, was perhaps truly hoping for the redemptive discovery of anaesthesia – Wells had had an opportunity to demonstrate his expertise with ether.
He had anaesthetised a patient awaiting a tooth extraction. The fact that the experiment had failed miserably, and the patient was screaming with pain, can be wholly explained now that we know more about physiology.
What is today an obvious physiological fact would have appeared 174 years ago to be an unimaginable, stupid theory, had there been any attempt at all to find out why, after Wells’s hundreds of successful anaesthesias, precisely that one, the Fateful one, had to fail.
Of course, it still does happen in medicine that, at far remove from any reasonable explanation, doctors defend obsolete dogma with swords drawn, or turn their backs as if deaf and blind to their colleagues’ successful, albeit not fully understood treatment results.
This seems to be hereditary in medical circles, where many would rather continue with destructive routine practices than to admit that, in the interests of healing, they could learn something newer and better.
That earlier patient was an alcoholic, who simply metabolised the ether faster, before the end of the operation. As Wells failed, Warren had smiled scornfully – hadn’t he said it is impossible to alleviate the pain?
On the big day, then, Gilbert Abbott (his face deathly pale, fearing his impending doom), the surgeons (with derisive smiles), and the medical students (grinning with Schadenfreude) observed as Morton began anaesthetising the patient using ether.
He held the glass container in the patient’s mouth for a good deal longer than Wells had previously, and urged Gilbert to take deep breaths. Then, he turned over the now flaccid patient to Warren, who folded up his sleeve and cut into the man’s body.
Anxious silence followed Warren’s every move, at any moment expecting the patient’s death rattle while he was coolly extracting the tumour, but there was nothing but deep, cosmic silence in the theatre. The scorn suddenly disappeared from Warren’s face, and his eyes filled with tears.
At the end of the operation, with his voice muffled and hoarse, he managed only a few words: “Gentlemen, this is no humbug.” He was almost beside himself at this experience, his haggard face wet with tears.
The present observers were deeply affected by the sight of tears on the face which for years had been unmoved by screaming patients whose flesh Warren was cutting and burning, and everyone there sensed that a breakthrough had just been achieved which shook the foundations of surgery at the time.
Effective anaesthesia enabled further progress which forever changed the results of operations.
Hitherto unseen advancements could be made, of which over thousands of years neither surgeons nor patients had dared to dream.
The European path
True, we in Europe were very slow to pick up anaesthesia compared to our American colleagues, who were already routinely using anaesthetics when over here there was still but debate over their necessity.
Thus Sir Robert Peel, a famous politician at the time, had to die a torturous death after suffering a riding accident which caused terrible bone fractures in 1850. Bone fragments had damaged several blood vessels, and he was bleeding heavily. Sir James Clark, court doctor of Queen Victoria, took him by carriage to Whitehall Garden, and called the leading surgeon in England for help.
This was five years after the discovery of anaesthesia in America, but due to sheer indecision not one doctor in England would make use of it. The patient was plagued by such pain that he could not even be touched, let alone bandaged. He agonised for three horrible days before he died.
In England the breakthrough had come on the 21st of December 1846, when Professor Robert Liston operated on Frederick Churchill, an exhausted butler dying of sepsis. Liston’s comment on the first operation using ether: “Let us try this Yankee trick, which can allegedly induce numbness”.

Instead of chanting praises whilst introducing it into surgical practice, only the controversy about whether or not to use pain relief intensified. It took a few more years for the steadfast believers of the old doctrines before they started applying this “Yankee trick” on a regular basis.
Unfortunately, at that time, as in many places today, these men had decision-making power. That is about life and death.
A new era, but no panacea
Thus began the century of surgery, with the belief that the barriers to surgery were gone, and the possibility of real choice had opened up for patients, who before could only choose whether to die of illness, or of surgery.
As after all ‘eureka’ moments in medicine, soon surgeons were astonished that this wasn’t the single, miraculous intervention they’d hoped for, since large numbers of patients continued to die in now painless operations due to sepsis or to shock from blood loss.
Further necessary steps, for which hundreds of doctors fought, were disinfection, handwashing, and hygienic conditions in hospitals.
It has been a long road of 174 years from conscious patients in agony during surgery to the appearance of ultramodern operating theatres, from where patients now have much greater chances of emerging alive.
Today, amongst other things, the emergence of antibiotic-resistant bacteria cautions against overconfidence. Every day 100-150 people die of sepsis in England alone, we today have no new breakthrough antibiotics like penicillin was 79 years ago.
The effect of humble penicillin was known for a thousand years, but since it was used by the very poor to treat inflammation, it was of course not taken seriously by serious science.
Until Flemming, that is, who by the way didn’t immediately recognise the significance of what had happened in his petri dishes. The medical form of penicillin was born a couple of years later, thanks to two other doctors.
There is space for – and it’s about time – holistically observing and approaching the human body during treatment, soberly trusting its self-healing capacities, and supporting these as much as possible with natural substances.
